Finger Joint Arthritis
When you stop to think about how much you use your hands, it’s easy to see why the joints of the fingers are so important. Arthritis of the finger joints has many causes, and arthritic finger joints can make it hard to do daily activities due to pain and deformity. Unbearable pain or progressive deformity from arthritis may signal the need for surgical treatment.
This guide will help you understand:
Anatomy
How do the finger joints normally work?
The bones in the palm of the hand are called metacarpals. One metacarpal connects to each finger and thumb. Small bone shafts called phalanges line up to form each finger and thumb.
The main knuckle joint is formed by the connection of the phalanges to the metacarpals. This joint is called the metacarpophalangeal joint (MCP joint). The MCP joint acts like a hinge when you bend and straighten your fingers and thumb.
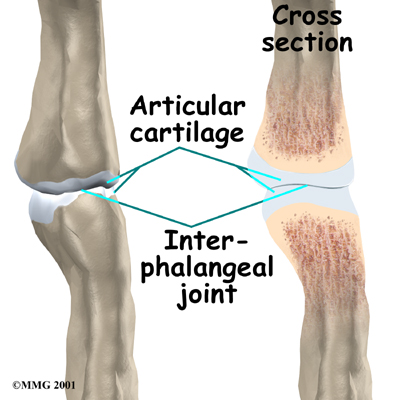
The three phalanges in each finger are separated by two joints, called interphalangeal joints (IP joints). The one closest to the MCP joint (knuckle) is called the proximal IP joint (PIP joint). The joint near the end of the finger is called the distal IP joint (DIP joint). The thumb only has one IP joint between the two thumb bones. The IP joints of the digits also work like hinge joints when you bend and straighten your hand.
The finger and thumb joints are covered on the ends with articular cartilage. This white, shiny material has a rubbery consistency. The function of articular cartilage is to absorb shock and provide an extremely smooth surface to facilitate motion. There is articular cartilage essentially everywhere that two bony surfaces move against one another, or articulate.
Causes
What causes arthritis?
Degenerative arthritis is a condition in which a joint wears out, or degenerates, usually slowly over a period of many years. Degenerative arthritis is usually called osteoarthritis. The term arthritis means joint inflammation (pain, redness, heat, and swelling). The term degenerative arthritis means inflammation of a joint due to wear and tear. You may also hear the term degenerative arthrosis used. Degenerative arthritis is usually called osteoarthritis.
Injury to a joint, such as a bad sprain or fracture, can cause damage to the articular cartilage. An injury to any of the joints of the fingers, even if it does not injure the articular cartilage directly, can alter how the joint works. After a fracture, the bone fragments may heal in slightly different positions. This may make the joints line up differently. When an injury changes the way the joint lines up and moves, force can start to press against the surface of the articular cartilage. This is similar to how a machine that is out of balance wears out faster.
Over time, this imbalance in the joint can lead to damage to the articular surface. Since articular cartilage cannot heal itself very well, the damage adds up. Eventually, the joint can no longer compensate for the increasing damage, and symptoms begin. The damage in the joint starts well before the symptoms of arthritis appear.
Symptoms
What does arthritis feel like?
Pain is the main problem with arthritis. At first, the pain usually only causes problems when you begin an activity. Once the activity gets underway, the pain eases. But after resting for several minutes the pain and stiffness increase. When the arthritis condition worsens, pain may be felt even at rest. The sensitive joint may feel enlarged and warm to the touch from inflammation.
In rheumatoid arthritis, the fingers often become deformed as the disease progresses. The MCP joints of the fingers may actually begin to point sideways (towards the little finger). This is called ulnar drift. Ulnar drift can cause weakness and pain, making it difficult to use your hand for daily activities.
Both rheumatoid arthritis and osteoarthritis can affect the IP joints of the fingers. The IP joints may begin to flex (bend) or hyperextend (over straighten), causing characteristic finger deformities. Swan neck deformity occurs when the middle finger joint (the PIP joint) becomes loose and hyperextended, while the DIP joint becomes flexed. When the PIP joint flexes and the DIP joint extends, a boutonniere deformity forms.
Both forms of arthritis can cause enlarged areas over the back of the PIP joints. These areas tend to be sore and swollen. They are known as Bouchard’s nodes . Osteoarthritis causes similar enlargements over the DIP joints, called Heberden’s nodes.
Diagnosis
How do doctors identify arthritis?
The diagnosis of arthritis of the finger joints begins with a history of the problem. Details about any injuries that may have occurred to the hand are important and may suggest other reasons why the condition exists.
Following the history, a physical examination of the hand and possibly other joints in the body will be done. Your doctor will need to see how the motion of each joint has been affected.
X-rays will be taken to see how much the joint has changed. These tests can help determine how bad the degenerative damage from the arthritis has become. The X-rays also help the doctor estimate how much articular cartilage is still on the surface of the joints.
Treatment
What can be done for the condition?
Nonsurgical Treatment
Treatment usually begins when the joint first becomes painful. This may only occur with heavy use and may simply require mild anti-inflammatory medications, such as aspirin or ibuprofen. Reducing the activity, or changing from occupations that require heavy repetitive hand and finger motions, may be necessary to help control the symptoms.
An injection of cortisone into the finger joint can give temporary relief. Cortisone is a very powerful anti-inflammatory medication. When injected into the joint itself, it can help relieve the pain. Pain relief is temporary and usually only lasts several weeks to months. There is a small risk of infection with any injection into the joint, and cortisone injections are no exception.
Rehabilitation services, such as physical and occupational therapy, play a critical role in nonoperative treatment of finger joint arthritis. A primary goal is to help you learn how to control symptoms and maximize the health of your hand and fingers. You’ll learn ways to calm pain and symptoms, which might include the use of rest, heat, or topical rubs.
A custom finger brace or splint may be prescribed to support the finger joints. These devices are designed to help reduce pain, prevent deformity, or keep a finger deformity from getting worse.
Range-of-motion and stretching exercises are prescribed to improve your finger movement. Strengthening exercises for the arm and hand help steady the hand and protect the finger joints from shock and stress. Your therapist will also go over tips on how you can get your tasks done with less strain on the joint.
Surgery
Fusion
A fusion (or arthrodesis) of any joint is designed to eliminate pain by allowing the bones that make up the joint to grow together, or fuse, into one solid bone. Fusions are used in many joints and were very common before the invention of artificial joints for the replacement of arthritic joints. Even today, joint fusions are still very commonly used in many different joints for treating the pain and potential deformity of arthritis. Fusions are more commonly used in the PIP or the DIP joints in the fingers. A fusion of these joints is far easier and more reliable than trying to save the motion by replacing the joint.
Artificial Joint Replacement
Artificial joints are available for the finger joints. These plastic or metal prostheses are used by some hand surgeons to replace the arthritic joint. The prosthesis forms a new hinge, giving the joint freedom of motion and pain relief. The procedure for putting in a new joint is called arthroplasty.
Rehabilitation
What should I expect following treatment?
Nonsurgical Rehabilitation
If you don’t need surgery, range-of-motion exercises for the finger should be started as pain eases, followed by a program of strengthening. Your therapist will work with you to obtain or create special finger splints or braces (mentioned earlier) when needed. The rehabilitation program advances to include strength exercises for the fingers and hand. Dexterity and fine motor exercises are used to get your hand and fingers moving smoothly. You’ll be given tips on keeping your symptoms controlled. You will probably progress to a home program within four to six weeks.
After Surgery
Your hand will be bandaged with a well-padded dressing and a finger splint for support after surgery. Physical or occupational therapy sessions may be needed after surgery for up to eight weeks. The first few treatments are used to help control the pain and swelling after surgery. Some of the exercises you’ll begin to do help strengthen and stabilize the muscles around the finger joint. Other exercises are used to improve fine motor control and dexterity of your hand. You’ll be given tips on ways to do your activities while avoiding extra strain on the finger joint.
The Basal Joint Arthroplasty
Over the past 20 years, Dr. Coleman adopted the technique illustrated above. This proved to provide excellent range of motion and stability of the thumb with a very quick rehabilitation. His concerns about sacrifice of the flexor carpi radialis tendon(one of only 2 wrist flexors) lead him to refine the technique by harvesting the tendon from one of a group of tendon strands used to extend the thumb. One of these could be harvested without sacrificing the function of the remaining 2 or 3 tendons.
This is not a new technique invented by Dr. Coleman, and various version of the technique have been described by others.
As opposed to some traditional orthopedic methods of placing patients in a cast for 6 weeks after surgery, Dr. Coleman’s method allowed for patients to simply wear a splint that could be removed periodically for hygiene, and wound care; and could be dispensed with, in 6 weeks. The incisions for harvesting the tendon were located in the dorsal aspect of the forearm where they were much less visible. The patient was also spared of the scars on the inside of the wrist which also carry the stigma of previous attempts at suicide by slashing their radial arteries.
Over the past 3 years, the use of allograft tendons (tendons harvested from other people) has become much more widely acceptable and safe, as techniques have now been developed to eliminate the risks of transmission of disease from the donator. Our experience has also shown that the function of these allografts can equal those of the patients’ own tissue after approximately 3 months, and the tissues will be completely incorporated with the patient’s blood supply.
For the past 2-1/2 years, Dr. Coleman has been investigating the use of allografts for his basal joint arthroplasties. This has been very successful, in that joint function remains excellent, and the patient is spared of any incisions to harvest tendon grafts.